A health worker uses an oximeter to monitor the pulse and oxygen saturation levels of a resident during a door-to-door survey to check for Covid-19 coronavirus symptoms at a low income neighborhood in Hyderabad on May 6, 2021. Noah Seelam/AFP via Getty Images hide caption
A health worker uses an oximeter to monitor the pulse and oxygen saturation levels of a resident during a door-to-door survey to check for Covid-19 coronavirus symptoms at a low income neighborhood in Hyderabad on May 6, 2021. Bone Densitometer

Listen to Short Wave on Spotify, Apple Podcasts and Google Podcasts.
During the COVID-19 pandemic, one measurement became more important than almost any other — blood oxygen saturation. It was the one concrete number that doctors could use to judge how severe a case of COVID-19 was and know whether to admit people into the hospital and provide them with supplemental oxygen.
But pulse oximeters, the device most commonly used to measure blood oxygen levels, don't work as well for patients of color.
"There's no doubt in my mind that this has led to people not getting care, not getting timely care, or even being sent home or staying home to die from COVID-19," says Noha Aboelata, a family practice physician at the Roots Community Health Center. Aboelata is a co-author on one of several studies that have shown inaccuracies in the device have led to patients of color not getting timely care.
One group trying to make a better, more equitable device a reality is led by Kimani Toussaint, a physicist at Brown University.
"I was surprised that, you know, in this day and time it was a persistent problem, especially since the pulse oximeter is such a ubiquitous tool for physicians," Toussaint says. "I assumed someone would have addressed this problem."
The inaccuracy of pulse oximeters is not a new problem. As early as 1976, scientists at Hewlett-Packard recognized that pulse oximeters needed to be calibrated to different skin tones. "Because skin pigmentation and other absorbers affect the measurement, the method is not capable of making absolute measurements," two scientists wrote in the company's journal at the time.
Despite this, the devices eventually made it to pharmacies, hospitals, and people's medicine cabinets.
"It basically was born out of being tested on a white population," says Usha Lee McFarling, a national science correspondent for STAT, who has covered pulse oximeters extensively. "They were tested in the eighties in a time when there was so little diversity in our clinical trials and testing."
Other scientists began picking up on the discrepancy as early as the 1990s, but it didn't break into the medical mainstream. The few papers on racial bias in pulse oximeters were not reaching medical textbooks or top tier journals.
Doctors were largely unaware that the device that was instrumental in their work was faulty. "This is just ubiquitous in my world. I wouldn't think of taking a pulse or a blood pressure without taking a pulse oximetry in my daily practice," says Dr. E. Jane Carter, a pulmonologist at Brown University.
Carter almost always has an oximeter in her pocket, but after hearing about Toussaint's work and the inequities that lead to it, she wanted to be part of the solution.
"It was just sort of appalling to me that I'd spent 30 years as a pulmonologist using oximetry both in the United States and in sub-Saharan Africa to make decisions and possibly not been making the right decisions for all of my patients," she says.
Despite retiring from most of her work recently, she's committed to one more project: Helping Toussaint design a new oximeter.
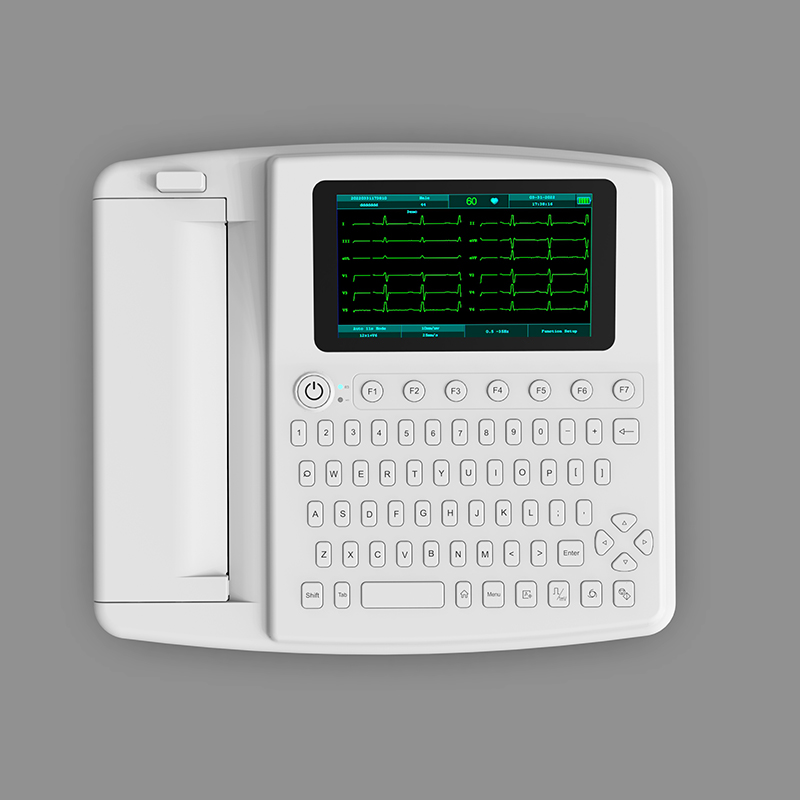
The pulse oximeter that most people use is a small device that clips onto a person's finger. The device shines two wavelengths of light into the finger. One wavelength is absorbed by oxygenated blood, and the other is absorbed by deoxygenated blood.
"Then we look at their relative absorption to take the ratio metric measure of how much one gets more absorbed than the other, and use that to estimate the amount of oxygen that is saturated in our blood," Toussaint says.
Pulse oximeters are known to be biased against darker skin tones. Kimani Toussaint is a physicist at Brown University working on an alternative to the pulse oximeter. Joshua Burrow/Kimani Toussaint hide caption
Pulse oximeters are known to be biased against darker skin tones. Kimani Toussaint is a physicist at Brown University working on an alternative to the pulse oximeter.
The oximeter then calculates what percentage of a person's blood has oxygen. But light is also absorbed by melanin, the protein that pigments skin. Because the devices were designed and calibrated using lighter skin tones, the melanin in people with darker skin causes the oximeter to overestimate how much oxygenated blood they have — and to underestimate how severe a case of COVID-19 is.
"Separating out the contribution of melanin, which would overlap with the contributions of oxygen deoxy hemoglobin, that is the challenge," Toussaint says.
But, he's trying a new approach. Instead of calibrating the same infrared technology on a diverse population, Toussaint is focusing on an entirely different property of light.
"We are trying to exploit the polarization or electric field properties of light," Toussaint says. "What we've been exploring is whether or not we can use this to differentiate the deoxy- from oxyhemoglobin — preferably at the same wavelength of light to minimize some of the other challenges of going across the spectrum and having different responses to melanin."
Toussaint is testing his shoebox-sized prototype in a hospital. This is where Carter, the pulmonologist, is lending her clinical knowhow. In practice, pulse oximeters are generally finicky — also thrown off by motion, nail polish, jewelry and placement.
Even if Toussaint's device works, it will take time to be approved and reach patients' fingers. In the meantime, doctors like Aboelata and Carter are using workarounds.
Aboelata has patients use an oximeter when they are healthy, creating a baseline to compare against when they are sick. But in situations where precise blood oxygen levels are high stakes – like admission to the hospital for treatment or approval for home oxygen to treat emphysema, Carter and Aboelata are turning back to the more difficult arterial blood gas test.
The test requires both a more difficult type of blood draw than most clinicians are used to and for the blood sample to be put into ice and immediately taken to a lab. This means that many clinics like Aboelata's can't even run the test. So if her patients need it she has to send them elsewhere. But, doctors also have to change the way they think of oximeters, she says.
"We'll have to either have a device that we know can be accurate for all skin tones or we'll have to go to another type of a test," she says.
Toussaint is hoping his polarization-based oximeter can be that test, so he can begin testing smaller models and companies can adopt his technology.
He feels the wide importance of his work and says strangers ask him for updates on his work. "That has really hit me — just how much impact that this work could have if it's successful," he says. "That, to me, is exciting. But I do also appreciate that significant responsibility is associated with that."
Listen to Short Wave on Spotify, Apple Podcasts and Google Podcasts.
Trolley Ultrasound The audio version of this story was produced by Thomas Lu and edited by Gabriel Spitzer. Neil Tevault was the audio engineer. Rebecca Ramirez edited the digital story. Anil Oza checked the facts.